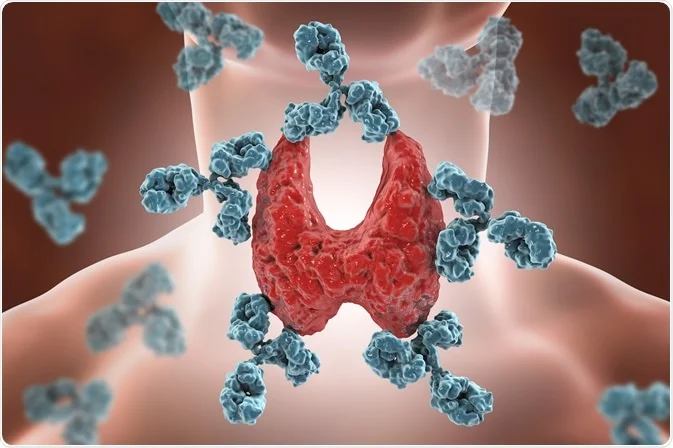
Recent advancements in the understanding and treatment of autoimmune disorders are offering new hope to millions of people worldwide. These disorders, in which the immune system mistakenly attacks the body’s own tissues, can cause chronic pain, fatigue, and a wide range of other debilitating symptoms. With innovative therapies and a deeper understanding of these conditions, the landscape of autoimmune disease management is evolving rapidly.
One of the most promising areas of research is the development of biologic therapies. These treatments, made from living organisms, target specific components of the immune system to reduce inflammation and prevent immune attacks on healthy tissues. Biologics such as TNF inhibitors, interleukin inhibitors, and B-cell inhibitors have shown significant success in treating autoimmune conditions like rheumatoid arthritis, psoriasis, and Crohn’s disease. These drugs offer more precise treatment options with fewer side effects compared to traditional immunosuppressants.
Advances in genetic research are also paving the way for more personalized treatment approaches. By identifying genetic markers associated with specific autoimmune disorders, researchers can develop targeted therapies that address the underlying causes of the disease. This precision medicine approach aims to tailor treatments to individual patients based on their genetic profiles, improving efficacy and reducing the risk of adverse effects.
Stem cell therapy is another innovative treatment showing promise in the management of autoimmune disorders. By harvesting and reinfusing a patient’s own stem cells, this therapy aims to reset the immune system and promote the regeneration of healthy tissues. Clinical trials are underway to assess the effectiveness of stem cell therapy in conditions such as multiple sclerosis, systemic lupus erythematosus, and type 1 diabetes. Early results are encouraging, suggesting that stem cell therapy could offer long-term remission for some patients.
Diet and lifestyle modifications are increasingly recognized as important factors in managing autoimmune disorders. Emerging research suggests that certain dietary patterns, such as the anti-inflammatory diet and the autoimmune protocol (AIP) diet, can help reduce symptoms and improve overall health. These diets focus on eliminating potential trigger foods and incorporating nutrient-dense, anti-inflammatory foods to support immune function and gut health.
The gut microbiome is also a key area of interest in autoimmune research. Studies have shown that an imbalance in gut bacteria can contribute to the development and progression of autoimmune diseases. Probiotics, prebiotics, and dietary interventions aimed at restoring a healthy gut microbiome are being explored as potential treatments. Fecal microbiota transplantation (FMT), which involves transferring healthy gut bacteria from a donor to a patient, is being investigated for its potential to reset the immune system and alleviate symptoms.
Holistic and integrative approaches to autoimmune disease management are gaining popularity as well. Integrative medicine combines conventional treatments with complementary therapies such as acupuncture, yoga, and mindfulness meditation. These approaches can help manage symptoms, reduce stress, and improve quality of life for patients with chronic autoimmune conditions.
Digital health technologies are also transforming the way autoimmune disorders are managed. Mobile apps and wearable devices enable patients to monitor their symptoms, track medication adherence, and connect with healthcare providers in real-time. These tools provide valuable data that can help personalize treatment plans and improve patient outcomes.
Despite these advancements, challenges remain in the diagnosis and treatment of autoimmune disorders. Many patients face long delays in receiving an accurate diagnosis due to the complex and often overlapping symptoms of these conditions. Increasing awareness and education about autoimmune diseases among healthcare providers and the general public is essential for early detection and intervention.
Access to advanced treatments and clinical trials is another critical issue. Efforts to expand access to cutting-edge therapies and ensure that all patients, regardless of geographic location or socioeconomic status, can benefit from the latest advancements are crucial for progress in this field.